
I spoke with cardiology regarding his EKG findings, who did not feel as though patient was a cardiac catheterization candidate at that time." I was able to visualize the ETT on initial intubation pass through the cords however given his continued hypoxemia, I felt it best to replace the tube to ensure no cuff malfunction or iatrogenic cause of his low O2.

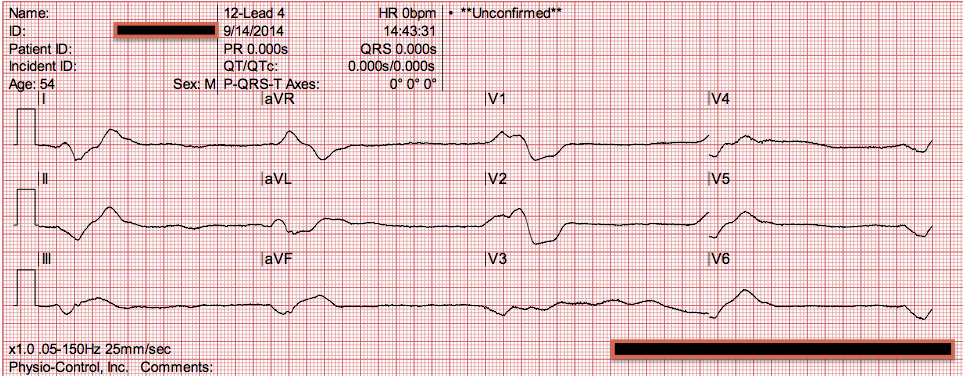
"Endotracheal tube re-intubation was confirmed multiple times, bilateral breath sounds, yet O2 saturation remained in the 50s and 60s. He had multiple cardiac arrests with ROSC regained each time. "Initial ROSC EKG showed what appeared to be in atrial fibrillation with inferior ST elevations, depressions in aVL, concerning for STEMI." Pulseless electrical activity with witnessed arrest as a predictor of sudden death from massive pulmonary embolism in outpatientsĬonclusions: outpatients with witnessed cardiac arrest and primary PEA carry a high probability of Massive Pulmonary Embolism When the ECG differential is between OMI on the one hand, and PE/type II OMI on the other, the absence of VT/VF strongly favors PE. Smith comment: Almost all witnessed arrest from OMI or any ACS is due to ventricular fibrillation and only about 5% of arrest from pulmonary embolism is due to ventricular fibrillation. "Looks like afib with subendocardial ischemia and right heart strain pattern." I sent it to 2 of my ECG nerd colleagues with no clinical information whatsoever, who instantly said: The morphology of V2-V4 is very specific in my experience for acute right heart strain (which has many potential etiologies, but none more common and important in EM than acute pulmonary embolism).

In addition to all of the above, there are T wave inversions in III and aVF, as well as T wave inversions in V2-V4. (The inferior ST depression vector of subendocardial ischemia counteracts the inferior component of the STE vector in all inferior leads except lead III, hiding the OMI).Īs in all ischemia interpretations with OMI findings, the findings can be due to type 1 AMI (example: acute coronary plaque rupture and thrombosis) or type 2 AMI (with or without fixed CAD, with severe regional supply/demand mismatch essentially equaling zero blood flow). This counteracts the STE of II and aVF, without affecting lead III. If this is ACS with Aslanger's pattern, the ST depression vector of subendocardial ischemia (due to simultaneous 3 vessel or left main ACS) is directed toward lead II (inferior and lateral). There is also STD in V2-V4 (but maximal in V5-V6). Thus, this apparently is Aslanger's Pattern (inferior OMI with single lead STE in lead III, with simultaneous subendocardial ischemia). In terms of ischemia, there is both a signal of subendocardial ischemia (STD max in V5-V6 with reciprocal STE in aVR) AND a signal of transmural infarction of the inferior wall with Q wave and STE in lead III with reciprocal STD in I and aVL. This is a complicated interpretation made even more so by the fact that it is immediately post ROSC. Initial ROSC was obtained, during which this ECG was obtained: It was reportedly a PEA arrest there was no recorded V Fib and no defibrillation. He reportedly told his family "I think I'm having a heart attack", then they immediately drove him to the ED, and he was able to ambulate into the triage area before he collapsed and became unresponsive. Written by Pendell Meyers and Peter Brooks MDĪ man in his 30s with no known past medical history was reported to suddenly experience chest pain and shortness of breath at home in front of his family.


 0 kommentar(er)
0 kommentar(er)
